Point-of-care HPV Molecular Diagnostics: Rapid and Precise Screening Test for Cervical Cancer
Cervical cancer is the fourth largest malignant tumor harmful to women’s health, with a grim prevention and control situation. Although cervical cancer has a serious disease burden, it is relatively more preventable and controllable due to its relatively clear etiology. In 2020, the World Health Organization (WHO) officially issued the Global Strategy for the Accelerated Elimination of Cervical Cancer, specifying the phased targets to be achieved by countries in the world in the areas of human papillomavirus (HPV) vaccination, cervical cancer screening and treatment in 2030.
With a relatively clear etiology, cervical cancer can be prevented and controlled through effective screening, early diagnosis and early treatment. On July 6, 2021, the WHO issued the latest guidelines for cervical cancer screening, which optimized the methodology and diagnosis strategy of cervical cancer screening and recommended HPV-DNA testing as the preferred screening method.
In the traditional three-stage model of screening, diagnosis and treatment, some abnormal populations failed to receive timely treatment due to loss of follow-up in each link, which reduced the prevention effect of screening programs. Therefore, the WHO has proposed the strategy of “treating immediately after screening” in its guidelines. Point-of-care HPV molecular diagnostics, as one of the keys to realize the strategy “treating immediately after screening” and characterized by high portability, simple operation and rapid testing, facilitates timely screening, and lays a foundation to realize the strategy of “treating immediately after screening”. The research team of Professor Zhao Fanghui from China National Cancer Center/Cancer Hospital of Chinese Academy of Medical Sciences published an article in the Chinese Journal of Preventive Medicine entitled Evaluation of the Effect of Point-of-care Screening Technology for Cervical Cancerto explore the point-of-care screening and testing of HPV and its effect on cervical cancer screening under the self-sampling and doctor sampling methods with the hybridization testing technology and conventional PCR method as the control.
The results showed that in the case of self-sampling, the overall consistency rate of HPV DNA testing and hybridization testing using POCT was 71.07%, the consistency rate with conventional PCR was 75.14%, and the kappa values were all 0.43, with medium consistency; in the case of doctor sampling, the coincidence rates of POCT with hybridization assay and conventional PCR were 81.68% and 79.85%, respectively, with kappa values 0.63 and 0.60, respectively. The above data showed that the results of the POCT had a medium consistency with those of the hybridization testing and the conventional PCR testing, and did not reach a high level. However, the authors also indicated in the research that this may be due to the different high-risk HPV types covered by different testing methods, and further researches may be required to compare the consistency between different research methods more accurately.
The screening effects of POCT, hybridization testing and conventional PCR for CIN 2+ were compared in the research. The results showed that, regardless of the sample type used, POCT (self-sampling: 0.742, doctor sampling: 0.779) had an AUC value greater than that of the traditional testing method using two sample types respectively, but the difference was not statistically significant; meanwhile, the AUC of POCT 16/18 typing using self-sampling and doctor sampling was optimal compared with conventional methods (self-sampling AUC=0.947, doctor sampling AUC=0.819), suggesting that the screening efficacy of POCT in predicting CIN 2+ was superior to conventional methods (hybridization testing and conventional PCR).
The performance of POCT using two different sample types was also compared. The results showed that the sensitivity and specificity of POCT for the testing of CIN 2+ in the self-samples were 100% and 28.95% respectively, while the sensitivity of POCT for the testing of doctor samples was 100% and the specificity was 55.85%; in testing the two types of 16/18 for the screening of CIN 2+, the specificity of self-samples could be increased to 89.74% with sensitivity unchanged, and when the sensitivity of doctor samples was decreased to 71.43%, the specificity could be increased to 92.45%. The results also showed that when CIN 2+ in histopathology was used as the disease endpoint, there was no significant difference in sensitivity and AUC between self-sampling POCT and doctor sampling POCT, but the specificity of self-sampling POCT was lower than that of doctor sampling POCT; in the testing of two types of 16/18, there was no statistically significant difference in sensitivity, specificity and AUC of self-sampling and doctor sampling methods. This result suggested that if the POCT results were shunted using the type 16/18 testing, the overall screening specificity could be improved, and the screening effect for cervical CIN 2+ lesion was good, and meanwhile, the testing performance of self-samples was not much different from that of doctor samples, and the specificity might be slightly impaired. The problem of insufficient specificity could be solved by testing two types of 16/18.
In summary, the results of this research showed that, compared with the hybridization testing and conventional PCR, the POCT testing performed in this research using the Sansure HPV test reagents had a higher accuracy in screening high-grade cervical epithelial lesions of CIN 2+, especially for type 16/18. Meanwhile, the specificity of the testing of 15 HPV types was low, and the screening specificity could be improved by shunting 16/18 type testing for patients with positive 15 type, thereby solving the problems of low specificity, excessive referral and excessive diagnosis and treatment for the existing HPV testing.
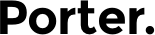
POCT had the advantages of short turnover of testing, convenience and practicality, without strict PCR laboratory partition settings and requirements. Its miniaturization, portability, and dispersibility were conducive to its application in areas with scarce medical resources, solving the blind areas in the application of large-scale diagnostic equipment, and improving the service ability of primary medical institutions. One of the challenges in cervical cancer screening in low-and middle-income countries is the availability and coverage of screening services. The urgency of molecular testing in the context of the COVID-19 epidemic has prompted secondary hospitals and county-level medical institutions with relatively weak medical conditions and no testing ability to rapidly improve their molecular testing capabilities, thereby laying a foundation for cervical cancer screening based on HPV testing. The POCT that is rapid and achieves testing in batches enables to complete the primary screening and treatment after abnormal primary screening on the same day, which makes it possible to treat immediately after screening advocated by the WHO.
Note: The picture comes from the Internet. If there is any infringement, please contact the author to delete it.
Disclaimer: All the publications on this website, where the source is indicated, are copyrighted by the original source and do not represent the position of this website.